Healthcare / Call Center / Sagility Bridgetowne
Polaris Careers
職位描述
1. Healthcare
- The Healthcare LOB focuses on providing end-to-end support to healthcare payers, providers, and members. Services include claims processing, member and provider support, prior authorization, benefits verification, and care management. The goal is to enhance operational efficiency and improve member satisfaction through accurate and timely healthcare solutions.
2. PCC (Provider Contact Center)
- The PCC LOB handles inbound and outbound communication with healthcare providers. Representatives assist with provider inquiries related to claims, authorizations, eligibility, payment status, and network participation. The focus is on delivering accurate information, resolving issues efficiently, and maintaining positive provider relationships.
3. HAP (Health Alliance Plan)
- The HAP process deals with servicing members and providers associated with the Health Alliance Plan. Responsibilities include assisting members with benefits, claims, coverage, and enrollment, ensuring compliance with HIPAA standards, and supporting the payer’s operational goals with high-quality customer service.
4. Dental
- The Dental LOB manages insurance-related services for dental care, including claims adjudication, benefits verification, and provider/member inquiries. The process ensures timely and accurate resolution of dental claims, adherence to policy guidelines, and quality communication with both providers and members.
5. BSC (Blue Shield of California)
- This process supports Blue Shield of California operations by handling member and provider interactions, claims support, eligibility verification, and issue resolution. The focus is on compliance, accuracy, and member satisfaction, aligned with BSC’s mission to provide accessible and affordable healthcare.
6. PPI (Provider/Payment Integrity)
- The PPI LOB ensures accuracy in payments and claim integrity by auditing claims, detecting overpayments or inconsistencies, and validating compliance with payer policies. It helps reduce financial leakage and supports regulatory adherence, safeguarding both payer and provider interests.
Requirements
- COLLEGE GRADUATE WITH OR WITHOUT BPO EXPERIENCE
- OPEN FOR 2 YEAR GRADUATE OR UNDERGRADUATE COMPLETED WITH 6 MONTHS WORK EXPERIENCE
- GOOD COMMUNICATION SKILLS
Other benefits:
- 20k Sign On Bonus
- 20% Night differential
- HMO coverage for employee upon Day 1 and HMO dependent upon certification
- Life and Accident Insurance
- Annual increase based on performance
- 13 and 14th month Pay
- retirement plan
- Virtual interview via msteams ( Final interview only 1 day process )
Castillo Jhon Eric
Talent Acquisition Specialists Polaris Careers
今天回覆 0 次
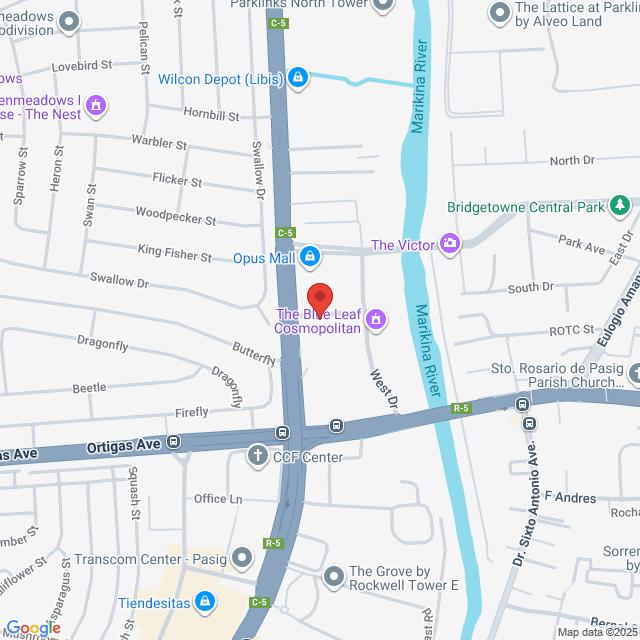
工作地址
Sagility Recruitment Hub. G/F Giga Tower, Bridgetowne, C-5 Road cor, Ortigas Ave, Quezon City, Metro Manila, Philippines
發布於 14 October 2025
猜你想看
查看更多Call Center Agent
 Neksjob Philippines
Neksjob PhilippinesHK$2-3.3K[月薪]
现场办公 - 奎松市無需經驗高中全職
Cyan NeksjobSourcing Specialist
Hiring for CSR Role With 20k Signing Bonus!
 Sagility Philippines B.V. Branch Office
Sagility Philippines B.V. Branch OfficeHK$2.5-3.1K[月薪]
现场办公 - 奎松市1-3 年經驗高中全職

Galapon JoelleRecruiter
Call Center Agent /College Graduate without Bpo Experience / Sagility Philipp...急招
 Polaris Careers
Polaris CareersHK$2.4-2.9K[月薪]
现场办公 - 奎松市<1 年經驗專科全職

Castillo Jhon EricTalent Acquisition Specialists
Call Center- Local Tagalog Account
 Sapient Global Services
Sapient Global ServicesHK$2.7-3.3K[月薪]
现场办公 - 奎松市無需經驗高中全職
Careers SapientRecruiter
Call Center Agent | Quezon City急招
 The Hird Corp.
The Hird Corp.HK$2.7-3.3K[月薪]
现场办公 - 奎松市無需經驗高中全職

Aquiles AmandaHR Officer

