Medical Claims Assessor
Eastwest Healthcare Inc.
職位描述
Key Responsibilities:
Claims Processing – Timeliness and Accuracy
- Review and process medical claims within the standard processing time.
- Ensure accuracy of approved amounts, encoding, and benefits of coverage in line with policies and member entitlements.
Daily Productivity Management
- Meet or exceed daily claims processing targets while maintaining high standards of accuracy and quality.
- Organize workload to ensure consistent processing volume and timely completion.
Compliance and Quality Assurance
- Ensure all processed claims comply with internal policies, medical necessity guidelines, and benefit limitations.
- Flag and escalate discrepancies, incomplete documents, or non-compliant claims for further review.
Data Entry and System Updates
- Accurately encode claims information into the processing system.
- Update claim statuses and resolution notes as required.
Internal Coordination
- Coordinate with internal department to clarify claim issues, seek approvals, or complete documentation.
- Provide support in resolving inquiries related to processed claims.
Continuous Improvement
- Recommend ideas for workflow improvement to reduce bottlenecks and increase efficiency.
- Participate in trainings and calibration sessions to stay updated with policy changes and system updates.
JOB QUALIFICATIONS:
Educational Attainment
- Bachelor's degree in Nursing, Allied Health, Business Administration, or any related field
- Associate degree holders with relevant experience may also be considered
Relevant Experience
- At least 1-2 years of experience in medical claims processing, health insurance operations, or related administrative/ healthcare roles
Areas of Experience
- Medical claims review and processing
- Health insurance or HMO operations
- Data entry and documentation
- Coordination with customers or internal stakeholders
Knowledge
- Basic understanding of medical terms, procedures, and diagnosis codes
- Knowledge of health insurance policies, benefits and claims guidelines
- Familiarity with medical necessity standards and benefit limits
- Proficiency in claims processing system and MS Office applications
Skills
- Strong analytical and decision- making skills
- High attention to detail and accuracy
- Good time management or organization skills
- Clear written and verbal communication
- Fast and accurate data entry skills
- Ability to stay focus during repetitive tasks
Competencies
- Commitment to compliance and quality
- Productivity and results- driven mindset
- Problem- solving and critical thinking
- Integrity and confidentiality
- Teamwork and collaboration
- Adaptability to changing processes
Licensure
- Not Required
- Nursing or medical-related licensure/certification is an advantage
Other Requirements
- Willing to work onsite and on shifting schedules
- Comfortable working with quotas, deadlines, and a fast-paced environment
- Open to training and continuous learning
Job Type: Full-time
Work Location: In person
Sanchez Edlyn
HR OfficerEastwest Healthcare Inc.
今天活躍
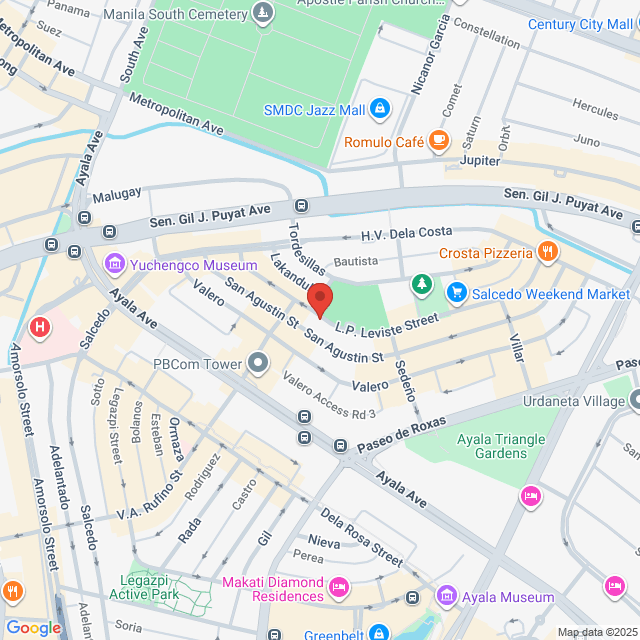
工作地址
6/F Makati Executive Center, V.A Rufino St., cor L.P Leviste St., Salcedo Village, Makati City, Salcedo Village Makati city
發布於 20 November 2025
猜你想看
查看更多Claims Support Role
 Mesco Express Service Corporation
Mesco Express Service CorporationHK$3.3-3.7K[月薪]
现场办公 - 馬卡蒂<1 年經驗本科全職

Diño NananVice President
Claims Supervisor
 Manila Bankers Life and General Assurance Corporation
Manila Bankers Life and General Assurance CorporationHK$4-5.3K[月薪]
现场办公 - 馬卡蒂3 - 5 年經驗本科全職

opg RecruitmentOwner
Claims Processor
 Paramount Life & General Insurance Corporation
Paramount Life & General Insurance CorporationHK$2.6-3.3K[月薪]
现场办公 - 馬卡蒂1-3 年經驗本科全職

hr renee.ursuaRecruiter
Claims Specialist
 SPD Jobs Incorporated
SPD Jobs IncorporatedHK$2.5-2.8K[月薪]
现场办公 - 馬卡蒂應屆畢業生/學生本科全職

Sombrio JannelleRecruitment Supervisor
Claims Specialist
 BPI MS Insurance Corporation
BPI MS Insurance CorporationHK$2-2.6K[月薪]
现场办公 - 馬卡蒂1-3 年經驗本科全職

Casidsid Andres IradHR Manager

