PHRN - Clinical Denials and Appeals
Gratitude Philippines
職位描述
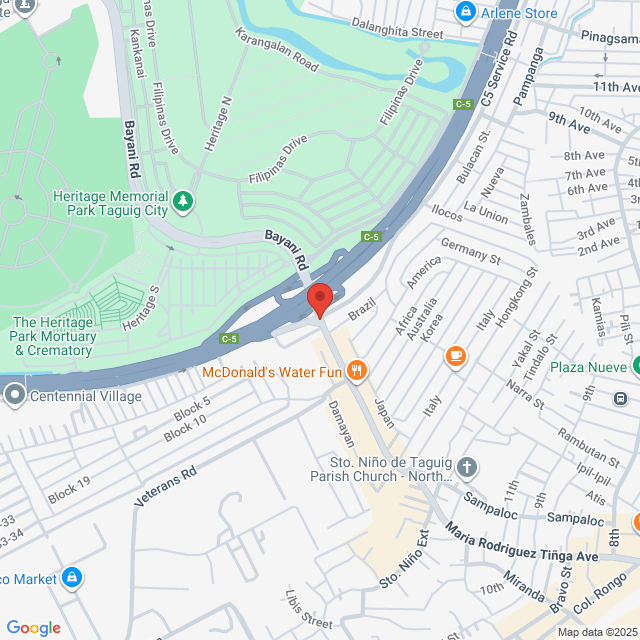
Work set up: Onsite Opportunity – MCK Taguig, Cyber Sigma Building
Work schedule :Weekdays Night Shift schedule, Fixed Weekends Off
- Effectively review inpatient and/or outpatient medical necessity and authorization denials to determine and understand the validity of such denials in a timely manner --Should conduct comprehensive reviews of the claim denial and account, to make determinations of what action to be taken to obtain reimbursement.
- Utilize payer policies, MCG and InterQual criteria to determine if account meets criteria for appeal
- Should write an appeal letter to payer using appropriate clinical indicators, citing Official Coding Guidelines, and documentation from within the patient's medical record
- Perform all other necessary steps on the specified accounts per Clients SOP’s including documentation in the EMR, including appeal package creation
- Manage the accounts until payment is received, the account is written-off, transferred to patient-liability, or other adjudication / movement within the system that is appropriate and agreed upon by both Parties
- Reporting quality results, tracking and trending of educational opportunities of the coding and CDI specialists, responding to client subject matter needs, and providing educational support and training
- PH Registered Nurse with experience in doing medical necessity appeals, lack of authorization appeals.(6 months needed)
- Proficient in reading Explanation of Benefits (EOB) and investigating denial root causes.
- Must be skilled in navigating various payer and provider portals.
- Typing speed of at least 45 WPM.
- Strong command of the English language, both spoken and written.
- Willing to work night shifts to communicate with payers.
- Familiarity with MCG and InterQual is a plus.
- Must NOT hold a USRN license
Afolabi Esther
Senior Talent Acquisition ConsultantGratitude Philippines
工作地址
Taguig
發布於 03 June 2025
猜你想看
查看更多Clinical Coordinator
 Zen Dental Spa and Aesthetic Center Corp.
Zen Dental Spa and Aesthetic Center Corp.HK$2-3.4K[月薪]
现场办公 - 達義<1 年經驗本科全職

VELMONTE JULIEHR Officer
Clinical Coordinator
 JLC EXPRESS MANPOWER CORPORATION
JLC EXPRESS MANPOWER CORPORATIONHK$4.7-5.4K[月薪]
现场办公 - 達義1-3 年經驗本科全職

Valencia BersalynLocal Manpower
Clinical Coordinator
 Creative Skin Medequip Inc.
Creative Skin Medequip Inc.HK$2.7-3.4K[月薪]
现场办公 - 奎松市應屆畢業生/學生本科全職

INC. CREATIVEHuman Resource
Clinical Coordinator
 Dempsey Resource Management Inc.
Dempsey Resource Management Inc.HK$2-2.7K[月薪]
现场办公 - 帕賽<1 年經驗高中全職

Dempsey HR VilmaTalent Acquisition Manager
Patient Coordinator-Cebu(based)急招
 Instalimb Solutions Philippines Inc.
Instalimb Solutions Philippines Inc.HK$2-2.7K[月薪]
现场办公 - 馬卡蒂1-3 年經驗本科全職

jose ma theresaHR/Admin. Manager

